Dry Eyes Explained: Causes, Symptoms, and When to See a Specialist
Dry Eyes, Specialist
Jul 2, 2025
•
4 mins read
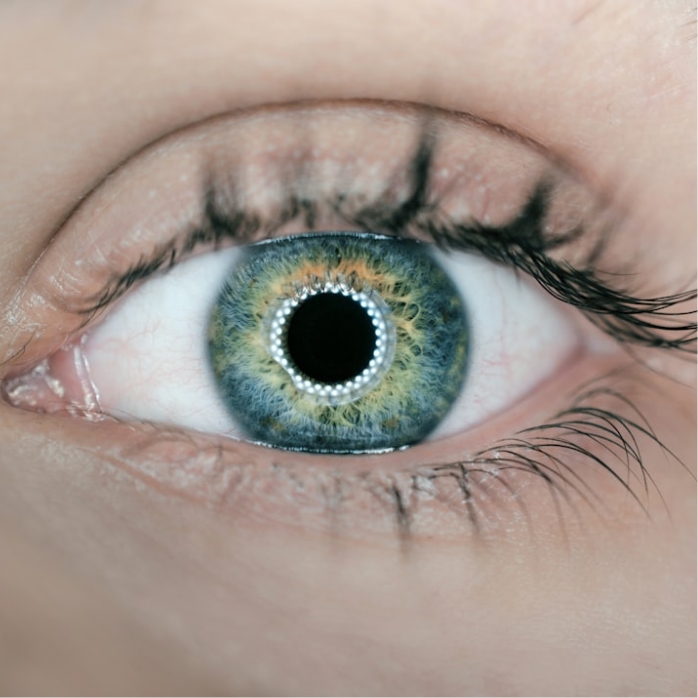
Ever felt like your eyes are gritty, burning, or just plain uncomfortable? You might be experiencing dry eye syndrome, a common condition that affects millions of people worldwide. While occasional dryness might just be a sign of a long day, persistent symptoms could indicate a chronic issue that requires attention. Understanding dry eyes – what causes them, how they feel, and when to seek professional help – is key to finding relief.
What Exactly Are Dry Eyes?
Our eyes rely on a healthy tear film to stay lubricated, nourished, and protected. This tear film isn’t just water; it’s a complex three-layer structure:
- Oily (Lipid) Layer: The outermost layer, produced by the Meibomian glands in your eyelids. It prevents tears from evaporating too quickly and makes the tear surface smooth.
- Watery (Aqueous) Layer: The thickest layer, produced by the lacrimal glands. It cleanses the eye and washes away foreign particles.
- Mucin Layer: The innermost layer, produced by goblet cells in the conjunctiva. It helps the aqueous layer spread evenly over the eye’s surface.
Dry eye occurs when there’s an imbalance in this tear film. This can happen if your eyes don’t produce enough tears (aqueous-deficient dry eye) or if your tears evaporate too quickly (evaporative dry eye). Most people with dry eyes have a combination of both.
Common Causes of Dry Eyes
The reasons behind dry eyes are varied and can range from lifestyle factors to underlying medical conditions:
- Aging: Tear production naturally decreases as we get older, especially after age 50.
- Environmental Factors: Dry, windy, or smoky climates, as well as air conditioning and heating systems, can increase tear evaporation.
- Screen Time: Prolonged use of computers, smartphones, and other digital devices reduces our blink rate, leading to increased tear evaporation.
- Medications: Certain drugs can reduce tear production, including antihistamines, decongestants, antidepressants, diuretics, and some blood pressure medications.
- Medical Conditions: Autoimmune diseases like Sjögren’s syndrome, lupus, and rheumatoid arthritis, as well as thyroid disorders and diabetes, can cause dry eyes.
- Eyelid Problems: Conditions like blepharitis (inflammation of the eyelids), meibomian gland dysfunction (MGD), or entropion/ectropion (eyelids turning inward/outward) can disrupt the tear film.
- Contact Lens Use: Wearing contact lenses can increase evaporation and irritation.
- Hormonal Changes: Menopause in women is a common cause of dry eye symptoms.
- Eye Surgery: Procedures like LASIK can temporarily reduce tear production.
Recognizing the Symptoms
Dry eye symptoms can range from mild annoyance to significant discomfort, impacting daily life. Common signs include:
- Stinging or burning sensation
- Gritty or scratchy feeling, like something is in your eye
- Redness of the eyes
- Sensitivity to light (photophobia)
- Blurred vision, especially after reading or screen use
- Feeling of heavy eyelids
- Difficulty wearing contact lenses
- Watery eyes (paradoxically, as the eye tries to compensate for dryness by producing reflex tears)
- Eye fatigue
When to See a Specialist
While occasional dry eyes can often be managed with over-the-counter remedies, there are times when it’s crucial to consult an eye care professional:
- Persistent Symptoms: If your dry eye symptoms don’t improve with basic measures (like artificial tears, taking breaks from screens) or worsen over time.
- Severe Discomfort: If the burning, stinging, or grittiness is significantly affecting your quality of life, sleep, or ability to perform daily tasks.
- Vision Changes: Any new or worsening blurred vision, especially if it doesn’t clear with blinking.
- Pain: If you experience sharp pain or a constant aching sensation in or around your eyes.
- Redness and Discharge: While some redness is common, if it’s accompanied by pus or a sticky discharge, it could indicate an infection.
- Suspected Underlying Condition: If you have an autoimmune disease, thyroid issue, or are taking medications known to cause dry eyes, it’s wise to discuss your symptoms with an ophthalmologist.
- After Eye Surgery: If you develop severe dry eye symptoms following refractive surgery or cataract surgery.
An ophthalmologist or optometrist can perform a comprehensive eye exam, assess your tear film, and determine the underlying cause of your dry eyes. They can then recommend tailored treatment plans, which might include prescription eye drops, punctal plugs, lifestyle adjustments, or in some cases, specific therapies for underlying conditions like MGD.
Don’t let dry eyes diminish your comfort or your vision. If symptoms persist, take the important step of consulting a specialist to find the right solution for you.
